POP Culture 101: It’s not what you think!
CLICK HERE for PDFs of the following story inspired by author Ann Hauprich's recent POP wellness journey, accompanied by a POP Quiz with obstetrician-gynecologist Dr. Charles Lasky and POP Culture 101 Homework Assignment prepared by urogynecologists Dr. David Kimble and Dr. Alexis Tran.
Pelvic Organ Prolapse education crucial to ending ignorance and shame which often delay treatment needed to prevent “out-of-body” experiences.
One might think a disorder that impacts millions of females from every hop, skip, jump and walk of life across North America would be a household word by now. Instead ignorance and shame top the long list of reasons why POP can needlessly progress to an advanced stage where it becomes disabling -- or even life-threatening. Little wonder the Bucket List of Ann Hauprich, whose first-person wellness story follows, now includes dreams of organizing a STOP POP movement. Those who join the campaign wouldn’t need to don pussy caps or march in rallies – although doing so might be a fun way to call attention to a serious health matter where the potential collateral damage spans far and wide. The decision to “bare all” was a difficult one for the author to make. However, the possibility that doing so might prevent even one female (be she someone’s daughter, mother, grandmother, aunt, cousin, niece, sister, spouse, mentor, neighborette, roommate, you-name-it!) from enduring a similar ordeal inspired her to press on.
My introduction to POP Culture 101 came the day before I was to undergo an operation commonly performed to silence the moans and groans of kidney stones.
Believing the rounded mass I’d discovered bulging in my pelvic region was a sign the pesky pebble slated for surgical removal had inflamed surrounding tissues and was struggling to pass on its own, I called my urologist’s office.
Perhaps I wouldn’t need to be wheeled into an operating room after all.
The relief that initially washed over me upon hearing the next day’s procedure would indeed be cancelled quickly turned to shock as the nurse announced: “What you’ve just described doesn’t sound like a kidney stone is passing. You need to contact a gynecologist. TODAY.”
Nothing could have prepared me for the reason. The protrusion -- combined with an escalating sensation of heaviness in my groin when upright -- were indications of POP: Pelvic Organ Prolapse. In other words, at least one of my pelvic floor organs was having an “out-of-body” experience. And as I was soon to learn, the exit ramp was none other than the passageway through which the last of my three babies had entered the world a quarter of a century earlier.
 My 65-year-old hands trembled as I searched for the
phone number of the practice where I had ceased booking annual pelvic exams
after recovering from a turn-of-the millennium hysterectomy. Why bother
taking time out from my jam-packed “sandwich generation” schedule to book an
examination that necessitated the use of gynecological stirrups when a
uterus and ovary were no longer to be found within?
My 65-year-old hands trembled as I searched for the
phone number of the practice where I had ceased booking annual pelvic exams
after recovering from a turn-of-the millennium hysterectomy. Why bother
taking time out from my jam-packed “sandwich generation” schedule to book an
examination that necessitated the use of gynecological stirrups when a
uterus and ovary were no longer to be found within?Why indeed! As my preliminary examination by obstetrician-gynecologist Dr. Charles Lasky and a second opinion by pioneering urogynecologist Dr. David Kimble would confirm, I had joined the ranks of a much misunderstood “POP culture” that impacts millions of females representing all ethnic, racial and socio-economic groups across the nation.
Like the majority of the one in four women who will experience some degree of POP in her lifetime, mine had gone undiagnosed and untreated for several years before I was referred to Dr. David Kimble, who distinguished himself as Chief of Urogynecology, Female Pelvic Reconstructive Surgery and Robotics at Albany Medical Center prior to co-founding the Women’s Center for Pelvic Wellness in Pasadena, CA with Dr. Alexis Tran (www.womenspelvicwellness.com).
And while ignorance and shame top the long list of reasons why females procrastinate in securing pelvic floor examinations, Dr. Kimble is adamant the disorder need not progress to the point where a portion of her bladder, uterus, bowel or rectum is bulging from her vagina.
Warning signs of POP, which can begin to develop as early as adolescence or as late as in postmenopausal years, run the gamut from stress incontinence to excruciating pain during sexual intimacy. And although childbirth and hysterectomies are common risk factors, even celibate nuns are not immune from developing the potentially physically, emotionally and spiritually debilitating condition.
Indeed Dr. Kimble believes boosting POP prevention awareness today could spare future generations the trauma of obliterative surgeries (where the vagina is narrowed or closed off to provide support for prolapsed organs) and/or complex pelvic reconstructive surgeries designed to restore normal organ functions. In my case the latter became necessary after my POP progressed to multi-compartmental Stage 3 of 4 – way too far gone for first-line non-surgical interventions. Foolish “Super Mom” heavy-lifting following two abdominal hernia repair surgeries and a major weight gain in the aftermath of myY2K hysterectomy and “no time” to do the recommended daily pelvic floor strengthening exercises ultimately necessitated a five-hour robot-assisted “sacrocolpopexy” that entailed repairing and creating durable support of the bladder (cystocele), rectum (rectocele) and the region that had once housed my uterus (apical prolapse).
The scope of the surgery (try to visualize 60-plus internal stitches in addition to several small external abdominal incisions) was necessary, according to Dr. Kimble, because leaving a single compartment unaddressed dramatically increases the risk of recurrent prolapse. Although it had been common in the past to only address the symptomatic compartment and leave all others in the original prolapsed state, it has since become evident this allows the untreated “weak link” to further prolapse and destroy the repair over time. Had I not undergone surgical intervention when I did, Dr. Kimble believes “the severity of the prolapse would have worsened to the point of complete protrusion of these organs permanently on the outside of the body. This condition, thereby, would eventually have caused obstructed constipation and obstructed urination with resultant renal failure.”
I shudder to think how close I might have come to having a different sort of “out-of-body” experience had Dr. Lasky not promptly referred me to Dr. Kimble. The importance of “hands on” pelvic examinations in addition to medical imaging cannot be over-stated since my own advanced POP failed to show up on the CT scan, ultrasound and X-ray. All three images that were done in the weeks prior to my POP diagnosis revealed a suspected kidney stone but failed to show my bladder was falling out of my body. (I never did end up having the operation that had been deemed necessary by my urologist. But that’s a whole other story!)
And while I still blush when talking about my POP surgery, my Bucket List now includes organizing a STOP POP movement. Those who join the campaign wouldn’t need to don pussy caps or march in rallies – though doing so might be a fun way to call attention to a serious health matter where as Dr. Kimble puts it “the potential collateral damage spans far and wide.”
Even medical professionals with patients who joke about “bashful bladders” and other urinary incontinence issues (“It was so funny, I peed my pants”) may benefit from reviewing the notes as a refresher course of sorts, says Dr. Kimble, who has operated on thousands of women with quality of life restoring outcomes. (POP is not to be confused with OAB, medical acronym for overactive bladder. To learn more about these and other urogynecological conditions treated by Dr. Kimble, please CLICK HERE.)
The fact that so many females – many still in young adulthood --are now sporting incontinence protection products is no laughing matter. However, the creators of modern feminine products are to be applauded for making even the most absorbent pads and disposable undies available in sleek designer styles that can pass skinny Jeggings detection tests.
I like to think readers who are drawn to related ads in magazines will pass the advertising messages along to friends and loved ones. Doing so might well become starting points for discussions with health care practitioners that could, in turn, lead to earlier detection of POP and other pelvic floor disorders.
Parting reflections plus a POP Quiz and
POP Culture 101 Homework Assignment
Ignorance and shame ultimately cost me the better part of a year of my life during which I was largely “UP-side down for the count” as my body, mind and spirit prepared for – and then healed from – a major reconstructive surgery to correct my advanced Pelvic Organ Prolapse. But the knowledge that further delays linked to ignorance and shame might well have led to renal failure – putting my very life on the line -- is beyond sobering.
The decision to “bare all” in this first-person essay was a difficult one to make. However, the possibility that doing so might prevent even one female (be she someone’s daughter, mother, grandmother, aunt, cousin, niece, sister, spouse, mentor, neighborette, roommate, you-name-it!) from enduring a similar ordeal inspired me to press on.
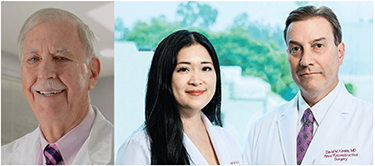 |
In the meantime, please click here to tackle a POP Quiz developed by Dr. Charles Lasky and click here for a POP Culture 101 Homework Assignment prepared by Dr. David Kimble and Dr. Alexis Tran to help females better understand and manage their pelvic health from adolescence to late post-menopausal years.
